Are your healthcare reform-related transformational changes on time and on budget? Are you seeing warning signs that some of the changes may stall, or take too long, or not drive sustained behavioral changes in important stakeholder groups, especially physicians? 
Here are 5 quick tips for dramatically increasing your chances for implementation "success."
1. Get alignment among senior leaders on what the definition of "success" really is.
It may sound really basic, but it's not unusual for us to talk to clients where senior level Sponsors are not aligned about what the scope of the change really is, and how they will measure the success of the implementation. Our measure of success, based on 30 years of change management consulting on major implementations, is:
- on time
- on budget
- all business, technical, and human objectives met
If you settle for anything less than these measures on your healthcare transformational changes you can be 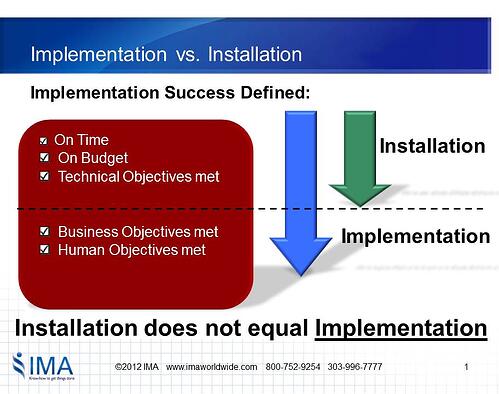 certain that you will not get the full benefit realization for your changes. You may "install" healthcare reform but won't get the associated sustained behavior changes which are essential to "implementation."
certain that you will not get the full benefit realization for your changes. You may "install" healthcare reform but won't get the associated sustained behavior changes which are essential to "implementation."
Installation and implementation are very different activities!
When you are "defining the change," you will need to have an elevator speech (what we call a Business Case for Action) at the "program" level. But-- this is not enough! You need to translate the Business Case for each major role group.
For example, for an ICD-10 implementation, you should have a specific Business Case for Action just for physicians. What's the change for physicians, why is it changing, and what happens if you are not success? ICD-10 is a compliance-based change so there is no choice-- it must be implemented.
But for many healthcare organizations there are transformational changes that are "commitment" based.
2. Identify how the change will impact different Target groups so you can anticipate the levels of resistance to the change.
It's particularly important to distinguish what the impact of the change will be for various "Target" groups. For example, if you are implementing ICD-10, what what will the change mean to the coders, what will the change mean to physicians, to finance, etc.
Once you know what the level of impact or what we call "disruption" will be, you will be able to prospectively determine the anticipated resistance to the change, since resistance is directly correlated to the amount of disruption.
Identification of these "human objectives" for each impacted role is critical to the ultimate success of the implementation. You'll see in a moment why these human objectives need to be defined by implementon-specific roles.
3. Make "active" Sponsorship of changes a top priority. Don't rely solely on steering committees as your Sponsors for healthcare transformational changes.
There is certainly nothing wrong with having a steering committee as part of your project governance structure. But the steering committee is not a substitute for active Sponsorship by leaders at all levels of the organization!
Even if you have a steering committee, you will need to build a "cascade" of Sponsors, at each level of management, and in all the areas impacted by your change. These Sponsors have 3 very important responsibilities:
1. They must express their personal commitment to the change.
2. They must model their personal and group commitment by what they are doing. We know that actions speak louder than words! These actions can include:
- Where they devote their time
- Where they allocate resources
- How they prioritize projects in their own areas of control
3. They must reinforce the new ways and make it harder to go back to old methods and practices. For example, if you are implementing EMR, are you making it easier for physicians to use the new system, and harder to go back to the old way of practicing? This reinforcement is 3 times more potent in driving behavior change than communication.
4. Given the importance of reinforcement, you must have "implementation-specific" reinforcements that are being applied frequently on "implementation-specific" measures to accelerate the change.
The more that you measure the specific behaviors associated with the change, and have leaders and managers apply "implementation-specific" reinforcements (positive and negative consequences), the faster your change will get implemented.
Process changes follow reinforcement. Simply put, people do what they are reinforced to do, by the individuals who have the greatest impact on their performance. No steering committee has the requisite positional authority that the manager of the individual has.
5. Develop a Change Agent network that is comprised of individuals with trust and credibility with Sponsors and Targets in operating groups at the local level. Technical project knowledge should not be the primary determining factor in selecting a change agent.
You can't throw a Change Agent who is an "unknown quantity" into an organization and expect to have a fully-productive Change Agent. Not only do you need sufficient numbers of Change Agents-- they have to be distributed based on the relationships they have with the people in that organization.
So, for example, if you have a Change Agent that is an expert in Epic, but has no previous relationships with physicians, that person will not be an immediately effective Change Agent with the physician population. Bottom-line: subject matter-expertise is not enough.
Follow these 5 tips and you will be better positioned to implement your healthcare transformational changes.