Mercy Healthcare is the 5th largest Catholic Healthcare System in the United States. They have facilities in 4 states and employ over 40,000 people. Between the Affordable Healthcare Act, plus sweeping clinical and operational changes, Mercy is typical of the crazy, busy world of healthcare today. In fact, they are a complex, innovative and forward-thinking organization that considers “change” a constant part of their lives. 
That said, they saw an opportunity to do better. Far too often, the change would be deemed complete, policies and processes changed, and communications sent--- then soon afterward people would go back to the old way of doing things.
Mercy was experiencing an all too common problem we call “installing a change” rather than “implementing it.” The changes are put into place, but behaviors don’t change. The fact is, you can install technology, processes, and new structures all day long, but nothing truly changes unless behaviors change {Tweet This}! And unless the behavior changes, you do not achieve full value realization for the investment of time, financial resources, and organizational energy made.
AIM: A Repeatable Process for the People Side of Projects
This revelation caused Mercy to look for a new, enterprise-wide change management framework. They recognized they needed a process for the people side of projects.
 Mercy narrowed their decision to two methodologies, but after attending an IMA Webinar led by Don Harrison, developer of the Accelerating Implementation Management (AIM) and doing a cost/benefit analysis, AIM stood out.
Mercy narrowed their decision to two methodologies, but after attending an IMA Webinar led by Don Harrison, developer of the Accelerating Implementation Management (AIM) and doing a cost/benefit analysis, AIM stood out.
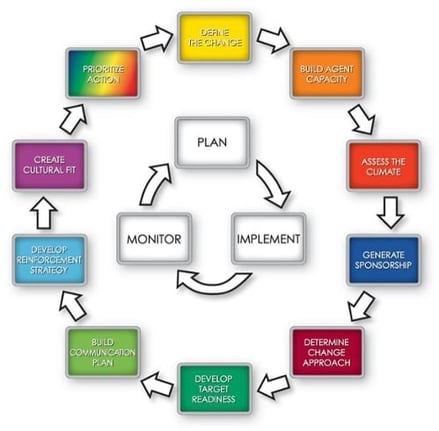
AIM consists of a set of ten core principles all of which integrate with the Project Management principles of Plan, Implement and Monitor. Although the Road Map shows the steps occurring in a linear fashion, the reality of complex change is that steps are repeated, or may occur in a different sequence. The methodology is essentially a set of principles, tactics, and strategies that are applied as needed. AIM is a perfect fit for Mercy’s needs.
As part of its methodology training and deployment, Mercy took a close look at their implementation history to get a data-based assessment of their implementation strengths and cultural challenges, and why their changes were not being sustained. This enabled them to pinpoint specific areas of focus.
Mercy’s Change Management Journey to Decentralize Scheduling
Once Mercy chose AIM as their change management methodology they piloted it on a few selected projects. The project team leaders were trained and a small core group of key individuals were AIM Accredited to provide the bench strength to coach others. One of these projects involved decentralizing the scheduling process in a clinic at one of the system sites. This had been attempted in the past without success. Here are several of the key AIM principles they used for the project:
Define the Change:
Mercy began with the perfect starting point for any change management project; they developed a clear, compelling definition of the change. Their Business Case for Action was as follows:
- What is changing? Patient calls to schedule appointments would no longer go to a central office. Instead the local doctor’s offices would book their own appointments.
- Why is it changing? To increase patient satisfaction and decrease the growing frustration by the doctors’ offices with the mistakes being made by the central office.
- What are the consequences if we don’t succeed? Patient and provider satisfaction would continue to decrease
Generate Sponsorship:
As Mercy knows, generating Sponsorship is the single most important success factor for any change project. They began by creating a Key Role Map to identify the CAST of characters for their change. This project deliverable documents all of the overlap between departments. It also identifies the Authorizing Sponsors who set the goals and resources for the project, and the Reinforcing Sponsors who need to demonstrate their personal commitment to the Targets. 
Develop Target Readiness:
To build readiness, Mercy conducted a Workflow Analysis with involvement from their Targets. They worked closely with all of the departments affected to re-distribute work. This ensured the staff in the doctor’s offices
that they would reasonably be able to take on the new task of scheduling. In this phase of the project they also considered and planned for all types of resistance.
Build Communication Plan
Mercy built a robust communication plan as seen here. Their communication methods were varied and included small groups, emails, memos and one-on-one meetings. They put careful consideration into every message and cascaded the messages throughout the organization in the frame of reference of each target audience.
Measuring the Business Results
So far, Mercy has been very pleased with the results of the implementation of their pilot project. Here are just a few statistics from their post project analysis:
- Visits are up 11%
- Front Desk Courtesy/Friendliness is up 5.3%
- Timeliness of scheduling is up 8% (this was a big struggle before)
- Call volume is down 1500/month (this is a huge result)
Mercy Healthcare’s goal was to build change capacity across their organization. They knew they needed to invest in a change management framework that could address highly complex changes that crossed multiple business units. IMA partnered with Mercy, not to “do it for them,” but to build their capacity to apply AIM on their own.
Watch this short video produced by Mercy on the real life benefits they achieved with AIM:
For a more in depth look at how Mercy selected and implemented AIM as well as the lessons they learned, click below to watch the one-hour webinar where our client contacts, Susan Duff, Director of Organizational Development; Dena Dishman, Manager of Talent Development; and Amber Wheeler, Director of Operations at the pilot site; talk candidly about Mercy Healthcare’s change management journey. It’s an excellent opportunity for you to learn from another organization’s experiences!